Genotype, which represents an individual’s genetic constitution, determines inherited traits and predispositions to genetic conditions such as sickle cell disease and thalassemia.
Similarly, blood group, classified by the ABO and Rh systems, governs the compatibility of blood transfusions and organ transplants while playing a crucial role in maternal-fetal health during pregnancy.
Recent advancements in genetic and hematological research have underscored the need for awareness and proactive management of these factors to enhance physical well-being and longevity. Beyond clinical implications, they also influence day-to-day decisions, such as choosing suitable partners for childbearing to avoid genetic complications, and understanding dietary requirements tailored to one’s biological profile.
This paper explores the intersection of genotype and blood group with quality of life, shedding light on how informed choices based on these factors can empower individuals to lead healthier, more fulfilled lives.
This exploration also highlights the role of education and healthcare systems in promoting awareness, equipping individuals with the knowledge necessary to leverage these biological determinants for better health outcomes.
By understanding the relevance of genotype and blood group, individuals can take proactive steps toward disease prevention, improved healthcare experiences, and overall quality of life enhancement.
Understanding Blood Genotype
Blood genotype refers to the genetic composition of an individual concerning specific hereditary traits. It is determined by the alleles inherited from both parents and plays a crucial role in defining various physiological and pathological characteristics.
Genotype is particularly significant in the context of hemoglobin structure, which influences the ability of red blood cells to transport oxygen efficiently throughout the body.
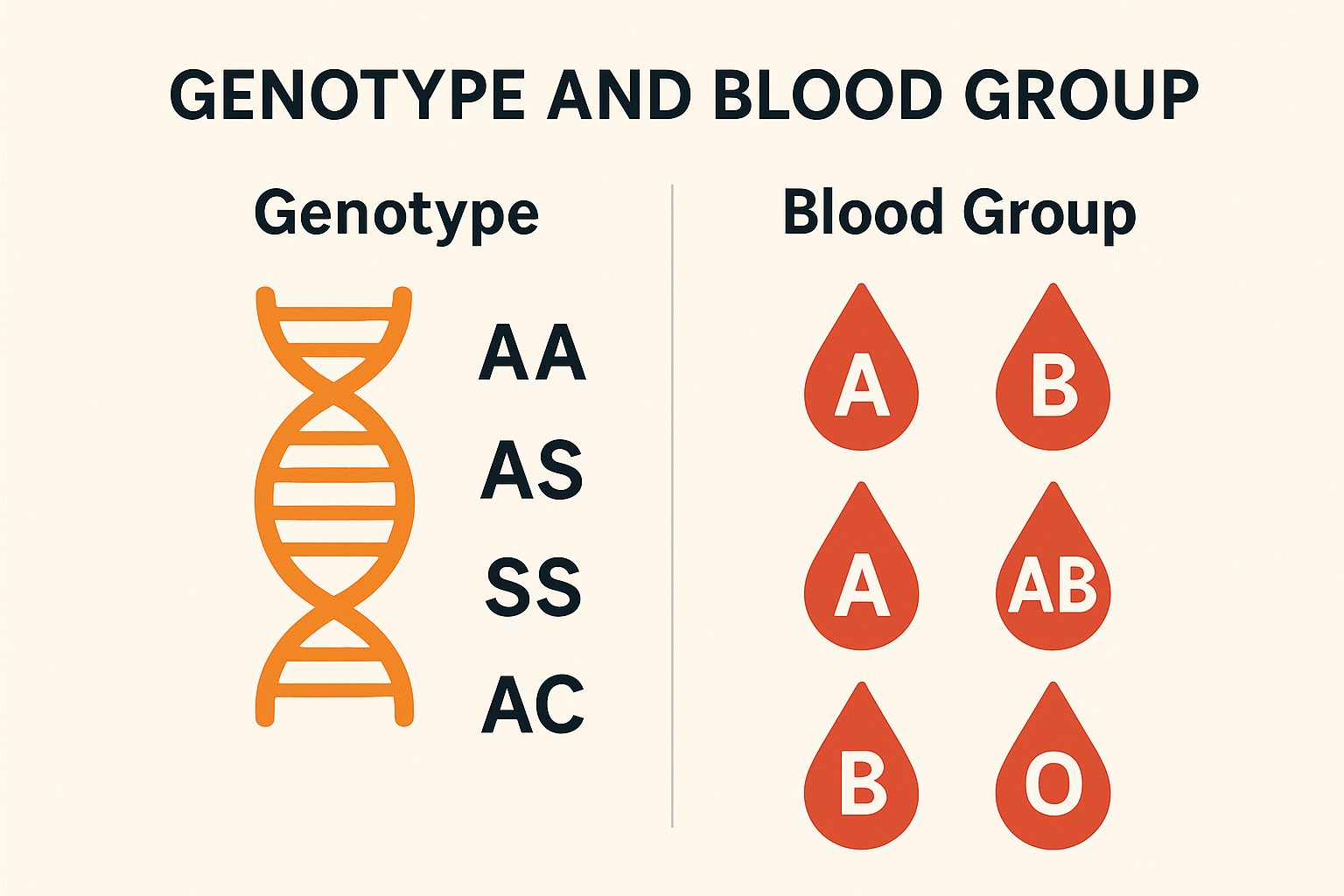
The most commonly discussed blood genotypes pertain to the hemoglobin gene, such as AA, AS, SS, and others. These classifications are essential for understanding an individual’s predisposition to genetic disorders, such as sickle cell disease (associated with the SS genotype) or sickle cell trait (associated with the AS genotype). These conditions arise from mutations in the beta-globin gene and can lead to significant health complications if not managed appropriately.
Understanding one’s blood genotype is integral to informed health management, particularly in regions where certain genetic conditions, such as sickle cell anemia, are prevalent.
Additionally, blood genotype knowledge is essential in premarital and antenatal counseling to prevent the transmission of severe genetic disorders to offspring.
As a key aspect of personalized medicine, blood genotype awareness enables individuals to make informed decisions that enhance their overall health and quality of life.
The Impact of Blood Genotype Awareness on Quality of Life
Understanding one’s blood genotype is a vital aspect of proactive health management and personalized medicine. Knowledge of an individual’s genetic composition enables informed decision-making, which significantly enhances their quality of life. Blood genotype awareness is particularly crucial in preventing, managing, and mitigating genetic disorders such as sickle cell disease, which is linked to specific genotypic combinations like SS or SC.
By identifying their blood genotype, individuals can take preventive measures to avoid health complications. For instance, those with AS or SS genotypes may adopt tailored lifestyle choices and medical interventions to minimize the risk of disease exacerbation.
Furthermore, genotype knowledge is essential in family planning, allowing prospective parents to assess potential genetic risks to their offspring and seek appropriate genetic counseling.
This awareness also facilitates better healthcare outcomes through personalized treatment plans. Healthcare professionals can design interventions that align with the genetic predispositions of patients, leading to improved disease management and reduced health risks.
Additionally, individuals with genetic vulnerabilities may engage in regular screenings and adopt healthy habits to preempt potential complications.
What Blood Genotypes Are Compatible?
The AA genotype has the best compatibility ratio. An individual with the AA genotype can choose a life partner from virtually all other genotype categories with an extremely minimal possibility of sickle-celled offspring.
Some research also shows that while the AA genotype is the best in terms of compatibility, it is also the most susceptible to malaria. So if you have the AA blood genotype, it is advisable that you minimize your exposure to mosquitoes and take other malaria prevention strategies seriously.
The AS genotype is best compatible with the AA. A genotypic pairing of AS with AS or AS with AC poses an increased chance of sickle-celled offspring. Similarly, a pairing between AS and SS or the AC and SS is equally as risky and ill-advised, while a pairing of two sickle-celled individuals will almost certainly result in sickle-celled offspring.
Interpretation of Blood Genotype Compatibility in Genetic Pairings
The compatibility of blood genotypes in reproductive pairings is a crucial consideration for reducing the risk of genetic disorders such as sickle cell anemia or hemoglobin C disease. Below is a detailed analysis of various genotype pairings and their implications:
AA + AS: Outcomes include AA, AS, AA, and AS. This pairing is considered Good, as there is no risk of offspring inheriting severe genetic disorders.
AA + SS: All possible outcomes are AS. This pairing is rated Fair, as the offspring will be carriers but will not develop sickle cell disease.
AA + AC: Outcomes include AA, AA, AA, and AC. This pairing is also rated Good, with minimal risk of severe genetic disorders.
AS + AS: Possible outcomes are AA, AS, AS, and SS. This pairing is rated Very Bad, as there is a 25% chance of producing offspring with sickle cell disease (SS genotype).
AS + SS: Outcomes include AS, SS, SS, and SS. This pairing is rated Very Bad, as the likelihood of offspring inheriting sickle cell disease is high (75%).
AS + AC: Possible outcomes are AA, AC, AS, and SS. This pairing is rated Bad, as the potential for offspring with genetic disorders (SS or AC genotypes) exists. Genetic counseling is advised.
SS + SS: All outcomes are SS. This pairing is rated Very Bad, as all offspring will inherit sickle cell disease.
AC + SS: Outcomes include AS, AS, SS, and SS. This pairing is rated Very Bad, due to the high likelihood of producing offspring with severe genetic conditions.
AC + AC: Possible outcomes are AA, AC, AC, and SS. This pairing is rated Bad, as there is a chance of producing offspring with sickle cell disease or other hemoglobinopathies. Genetic counseling is strongly recommended.
Advancements in the Treatment of Abnormal Blood Genotypes
For decades, abnormal blood genotypes, particularly those associated with sickle cell disease, were considered incurable and severely debilitating. However, significant advancements in medical research since the 1980s have unveiled promising treatments, with bone marrow and stem cell transplants emerging as potential cures.
A bone marrow transplant, the only established curative procedure for sickle cell disease, involves replacing defective stem cells in the bone marrow with healthy cells from a compatible donor, typically a sibling. This process restores the bone marrow’s ability to produce normal red blood cells, effectively eliminating the underlying cause of the disease.
Despite its potential, this treatment is not without challenges. The procedure carries substantial risks, including complications from immunosuppression, graft-versus-host disease, and infection.
Additionally, finding a suitable donor and the high cost of treatment further limit its accessibility, especially in low-resource settings and developing countries.
While bone marrow transplants hold immense promise, their limited application underscores the need for continued research and innovation. Expanding access to safer and more affordable curative therapies remains a priority in the global effort to combat abnormal blood genotypes and improve the quality of life for affected individuals.
Understanding Blood Groups
Blood groups refer to the classification of human blood based on the presence or absence of specific antigens on the surface of red blood cells.
These antigens play a crucial role in immune response and determine the compatibility of blood for transfusions, organ transplants, and other medical procedures. The two primary systems used for blood grouping are the ABO blood group system and the Rhesus (Rh) factor.
In the ABO system, blood is categorized into four main groups: A, B, AB, and O. These groups are defined by the presence of antigens known as A and B on the surface of red blood cells. Individuals with blood group A have A antigens, those with group B have B antigens, individuals with AB blood have both A and B antigens, and those with blood group O have neither A nor B antigens. The compatibility of these groups is vital in blood transfusion, as transfusion of incompatible blood can result in severe immune reactions.
The Rh factor further categorizes blood into Rh-positive (presence of RhD antigen) or Rh-negative (absence of RhD antigen). This classification is particularly important in prenatal care, as Rh incompatibility between a mother and her fetus can lead to complications such as hemolytic disease of the newborn if not properly managed.
Understanding blood groups is essential not only for medical purposes but also in forensic science, anthropology, and paternity testing. The ABO and Rh systems remain foundational to the practice of medicine, ensuring safe and effective healthcare delivery in transfusions, organ donations, and maternal-fetal health.
The Scientific Basis of Blood Group Compatibility
Blood group compatibility plays a pivotal role in ensuring the safety and efficacy of transfusion medicine. This compatibility is determined by the antigens present on red blood cells and the antibodies found in plasma, which interact to prevent adverse immunological responses during transfusions.
Red Blood Cell Compatibility
The compatibility of red blood cell transfusions is governed by the ABO and Rhesus (Rh) systems:
Individuals with A+ blood group can receive red blood cells from donors with A+, A−, O+, and O− blood types.
Those with A− blood group are limited to A− and O− donors due to the absence of the Rh factor.
For recipients with B+ blood group, compatible donors include B+, B−, O+, and O−.
Similarly, B− recipients can only accept red blood cells from B− and O− donors.
The AB+ blood group is unique as it can accept red blood cells from all blood types (A+, A−, B+, B−, AB+, AB−, O+, O−), earning it the designation of a universal recipient.
Conversely, AB− individuals can only receive from AB−, A−, B−, and O− donors.
The O+ blood group is compatible with red blood cells from O+ and O− donors.
O− individuals are universal red blood cell donors but can only receive from O− donors due to their lack of antigens.
Plasma Compatibility
Plasma compatibility is determined by the presence or absence of antibodies in the plasma:
A+ recipients can accept plasma from A+, A−, AB+, and AB− donors.
A− individuals are restricted to plasma from A− and AB− donors.
B+ recipients are compatible with plasma from B+, B−, AB+, and AB− donors.
B− individuals can receive plasma only from B− and AB− donors.
The AB+ blood group is a universal plasma recipient, capable of receiving plasma from all blood types due to the absence of anti-A and anti-B antibodies.
AB− recipients can accept plasma from AB− donors exclusively.
O+ individuals may receive plasma from O+, O−, A+, A−, B+, B−, AB+, and AB− donors.
O− recipients are compatible with plasma from O−, A−, B−, and AB− donors.
Clinical Significance
Blood group compatibility is fundamental to transfusion safety. Mismatched transfusions can trigger severe immune responses, including hemolysis and organ failure. Individuals with O− blood are universal donors for red blood cells, while those with AB+ plasma are universal plasma donors, enabling their use in emergencies.
Ensuring compatibility requires precise blood typing and crossmatching, underscoring the importance of advanced diagnostic technologies and adherence